Ethical and Legal Considerations for a COVID-19 Safe Psychotherapy Practice
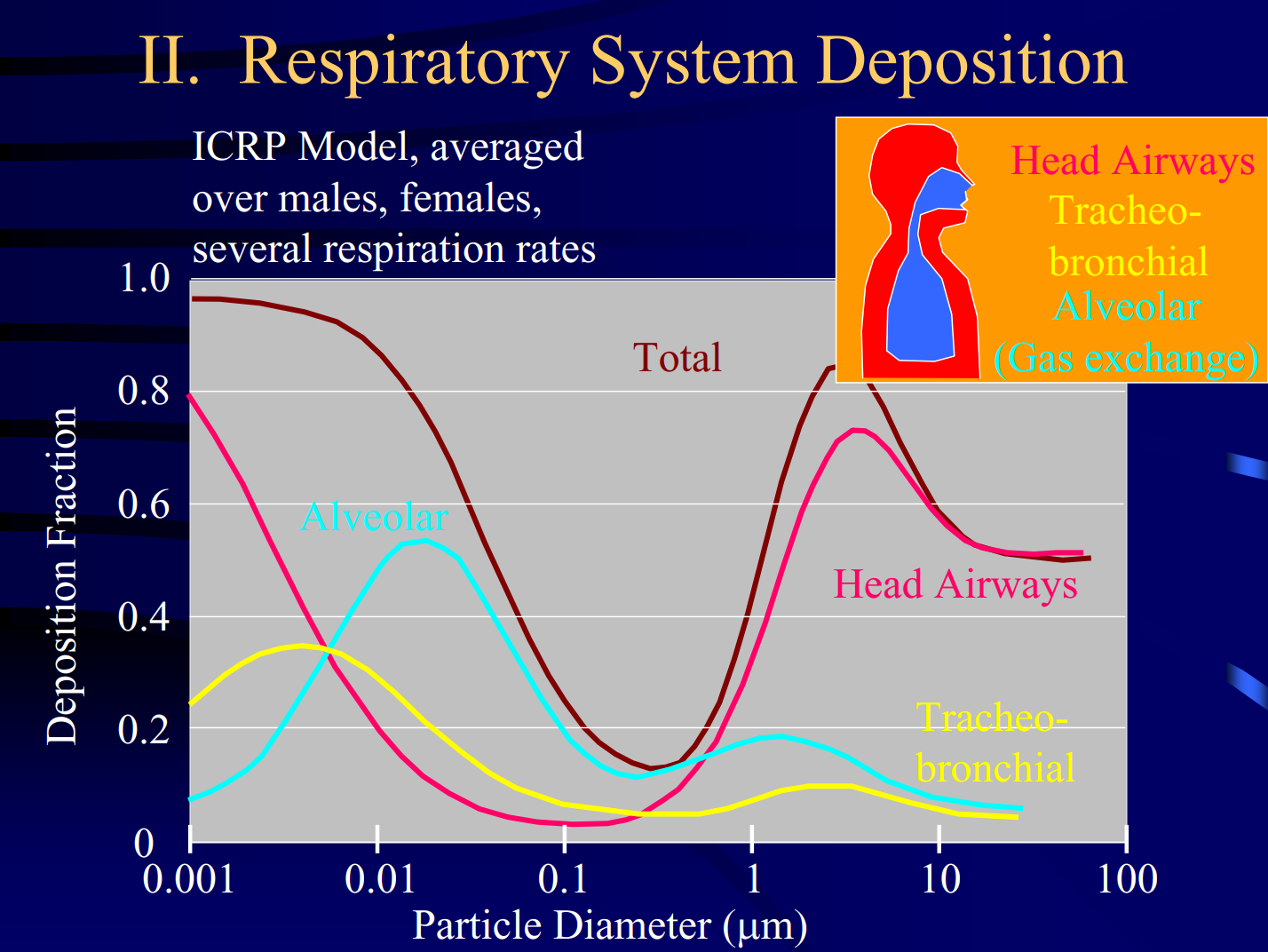
Did you know that the quantity of SARS-CoV-2 nuclei and droplets deposited in our airways and lungs are a fraction of the amount you breath and is a function of size.
Revised: March 23, 2021
Mentor Research Institute (MRI) has received guidance requests from mental health professionals including psychologists, counselors, and social workers. The article below responds to some questions and summarizes conversations.
The majority of psychotherapy, counseling and assessment services are provided by four disciplines. The term psychotherapist as used here includes (1) psychologists, (2) licensed clinical social workers, (3) licensed professional counselors, and (4) licensed marriage and family therapists.
What is a COVID-Safe office for psychotherapy practice?
For your consideration, a COVID-Safe office for psychotherapy practice is defined to include a licensed psychotherapist, any staff, an office and building that has been methodically evaluated in the light of relevant guidelines, physical characteristics, and mechanical requirements. The practice should have safety policies, procedures, and practices based on knowledge obtained through qualified education, training and/or consultation.
What are the compelling COVID-Safe ethical considerations facing psychotherapists during a pandemic?
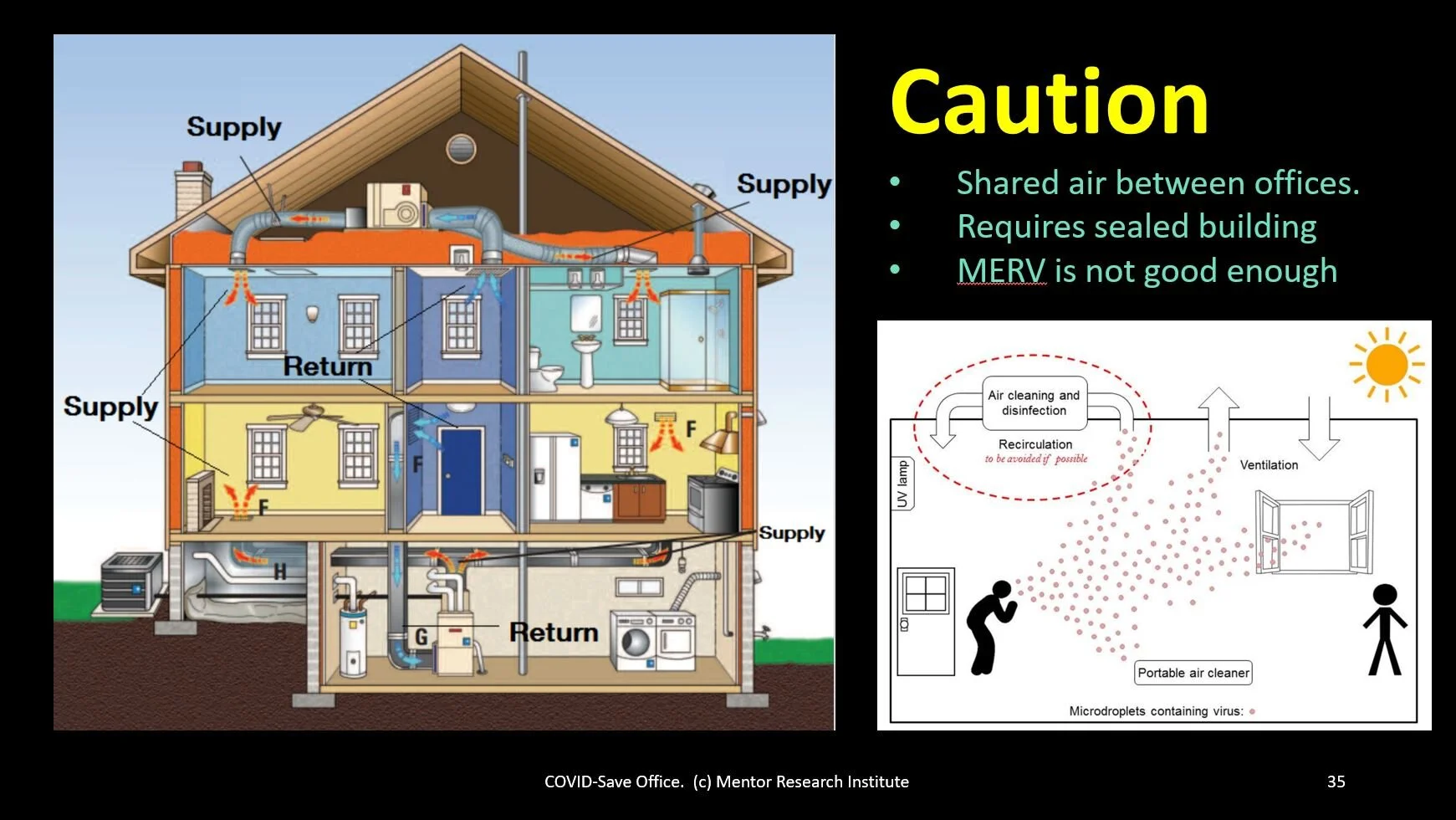
Did you know that offices that are rooms located in older home generally share air to a greater extent than modern offices. The ducting and filtering is not designed to meet medical standards for airborne infectious diseases.
In order to serve the public ethically, professionals adhere to similar and differing legal, ethical and professional responsibilities. Licensing Boards enforce ethical principles and guidelines of the several professional organizations. MRI proposes the following considerations as aspirations for all psychotherapists, their employees or employers.
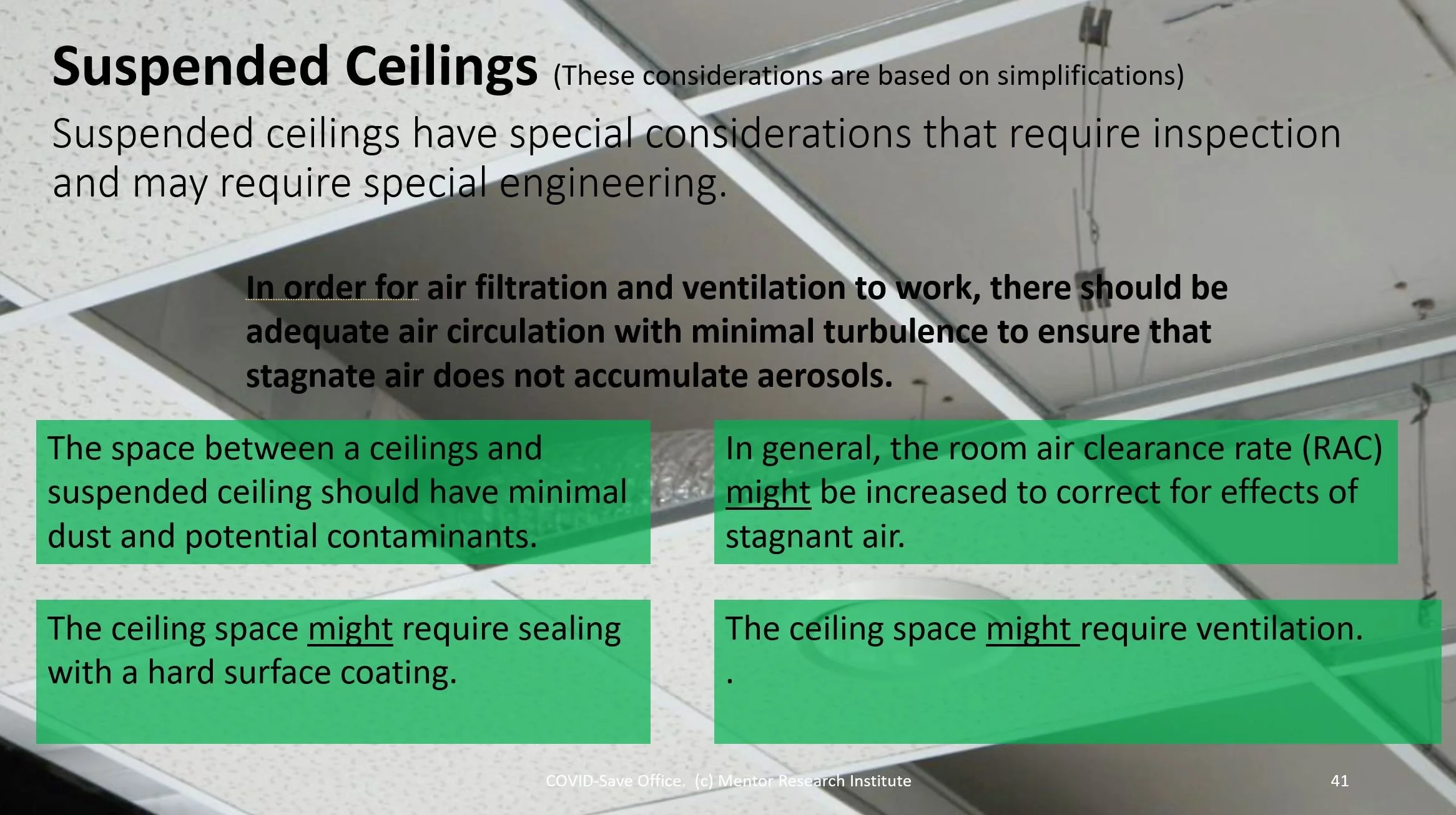
Suspended ceiling may require inspection for numerous potential problems and may require special engineering.
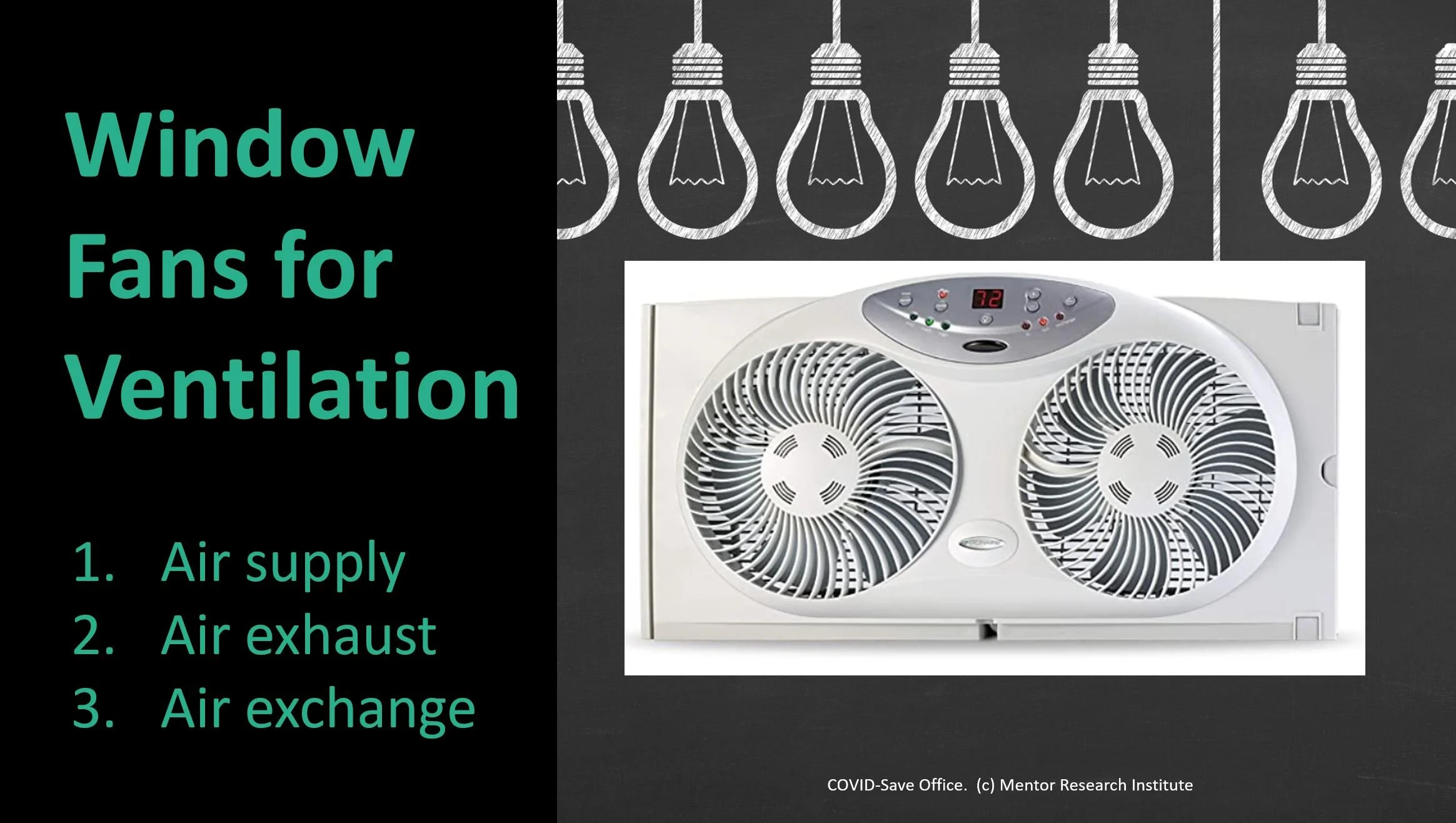
Did you know that an air supply window fan and an air exhaust fan properly placed at opposite ends of a room might be able to clear well mixed non-turbulent air at a rate of 100 to 200ft3/min? The air-exchange should be balanced for negative pressure.
Psychotherapists should obtain knowledge of the physical and operational considerations necessary to create and maintain COVID-Safe offices for psychotherapy and evaluation.
Psychotherapists will use science and evidence-based models to establish good safety practices. Psychotherapists should revise their practices as necessary if SARS-CoV-2 becomes a persistent public health issue.
Psychotherapists should obtain training that includes the terminology, concepts, technology, and methods necessary to discuss COVID-Safety with patients, colleagues, office-building owners, attorneys, licensing boards and third-party payers.
Psychotherapists should maintain an office environment which meets physical requirements, carefully implementing policies and procedures for office and building safety, source control, risk reduction, sanitization, air quality, and provide initial and pre-session screening, patient education, and informed consent.
Psychotherapists who offer advice or opinions to patients, colleagues or the public about COVID-Safe practices should be qualified. Civil law and ethical guidelines expect professionals to practice within their areas of competence.
Psychotherapists should understand the science behind relevant COVID-Safe office recommendations especially those that may be true in general but may not apply to their office, practice environment, local disease prevalence, or the needs of patients with specific health vulnerabilities.
Unless psychotherapists have a qualified health and safety staff member held responsible to maintain their COVID-Safe office, they need to be knowledgeable and to implement the policies and standards necessary to create and maintain a COVID-Safe environment.
If a psychotherapist intends to see patients with health vulnerabilities in their practice, they should seek qualified consultation or training that will inform their decisions about what is possible and necessary to see those patients within reasonable safety standards.
Psychotherapists should evaluate whether to see a patient in-person or use telehealth. Such evaluation and re-evaluation should be an ongoing process.
What should psychotherapists look for when seeking training or consultation regarding a COVID-Safe office?
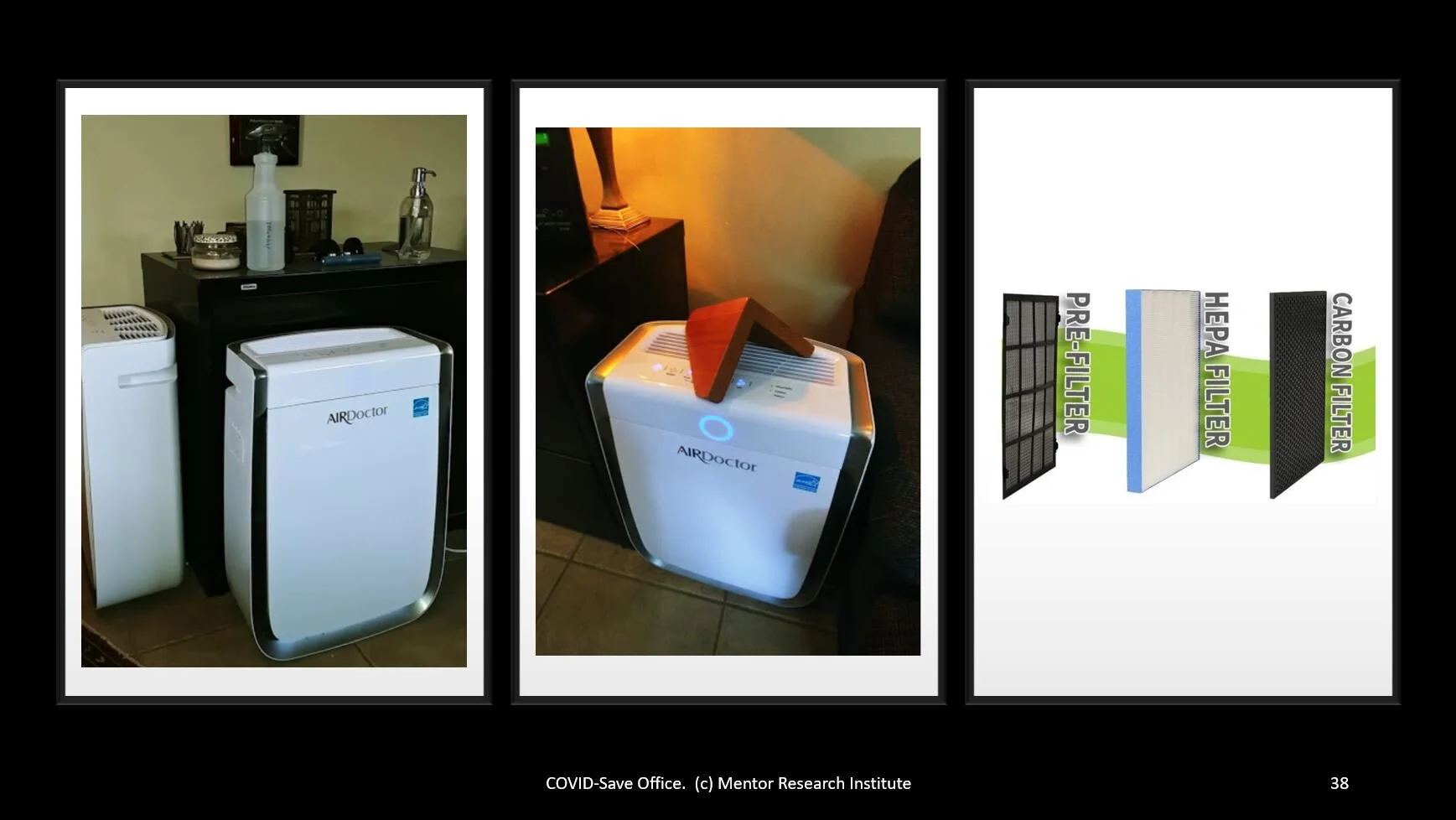
Did you know that there are 3 levels of HEPA filtration and that up to 99.997% of SARS-CoV-2 virus are trapped and killed. Additionally, a trust of 180ft/min can also kill any escaping virus subjected to impaction, desiccation and/or wind shear.
To establish a COVID-Safe office, psychotherapists should understand the characteristics of their office space and building, patients, and practices while considering relevant factors and concepts related to air quality and treatment.
Those qualified to provide group training and/or consultation regarding COVID-Safe office behavior should have deep understanding of the following variables, provide examples, and be capable of offering dynamic explanations:
office and building safety
source control
risk reduction
sanitization
air quality and treatment
initial and pre-session screening
patient education, and
informed consent
Those qualified to provide group training and/or consultation regarding COVID-Safe air quality have deep understanding of the following variables and are capable of offering dynamic explanation:
HEPA, TrueHEPA & ultraHEPA
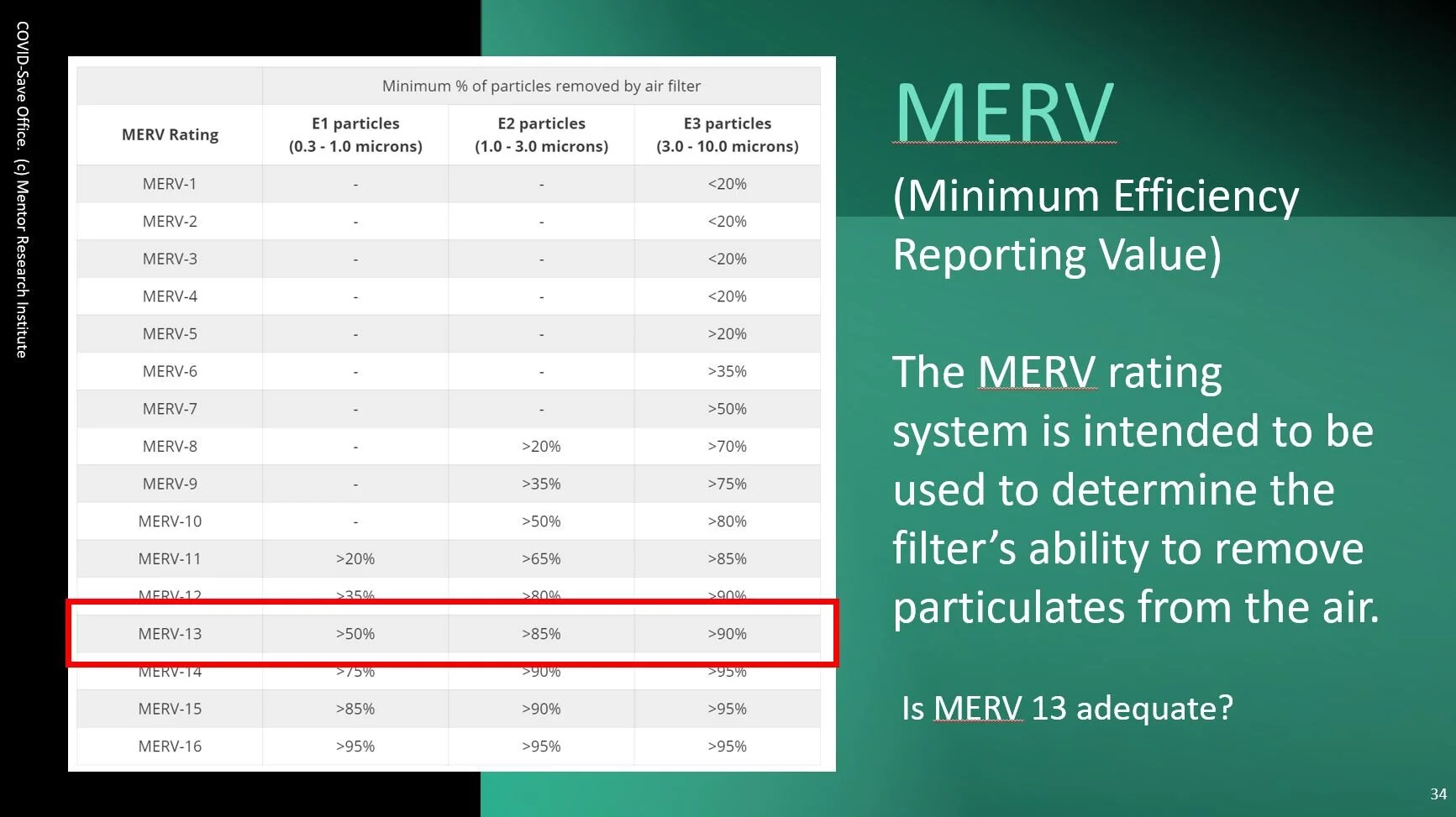
MERV 7 & MERV 13
safe office design
office volume
breathing tidal volume
air dilution & air treatment
air-exchange
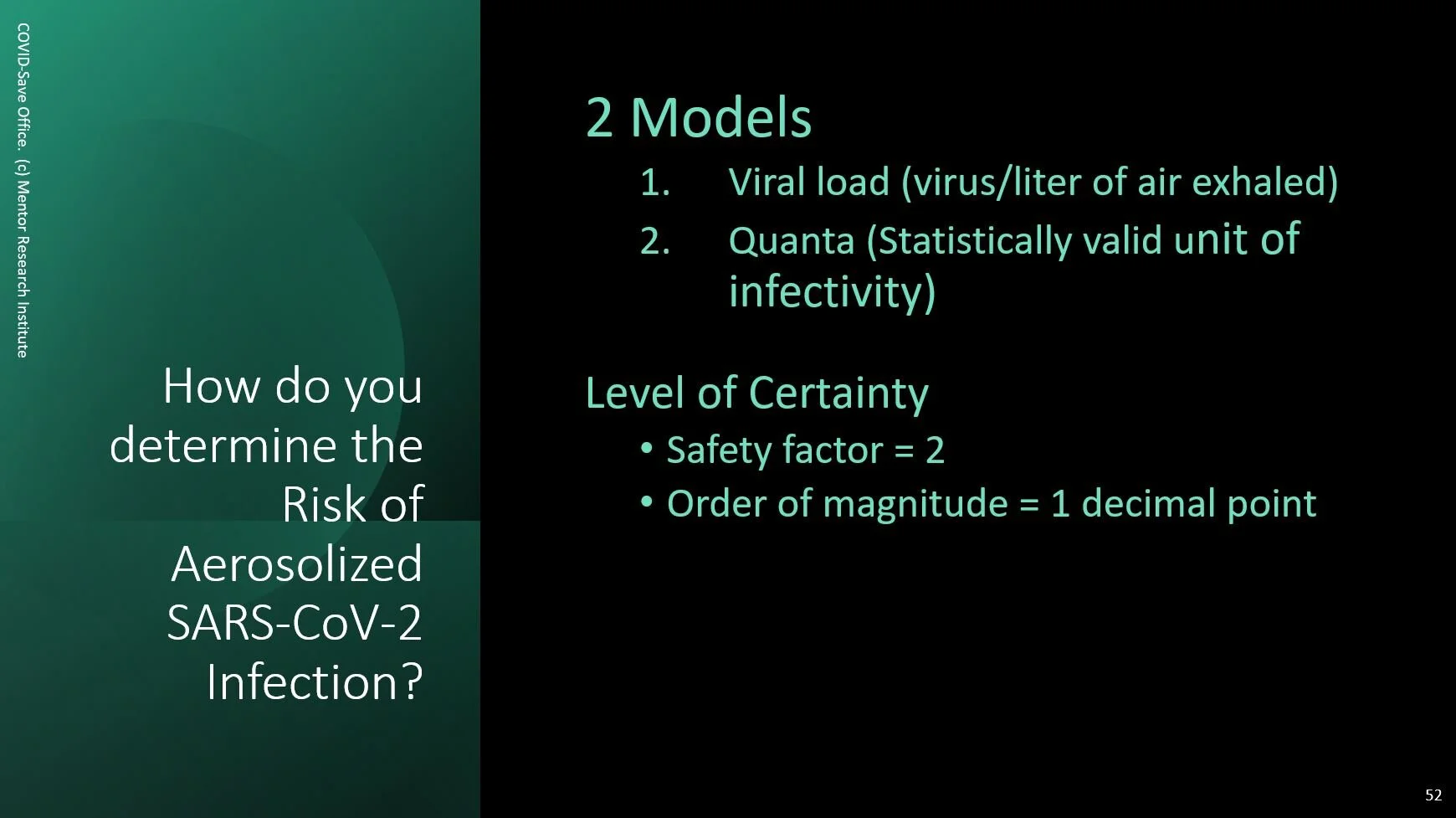
viral load and quanta
SARS-CoV-2 biological vulnerabilities
dissection, wind shear and impaction
SARS-CoV-2 half-life
room air clearance rate (RAC)
clear air delivery rate (CADR)
airborne infectious disease standards
physician’s exam room air quality standards
ratio of viral load to decibels
CO2 monitoring
particle monitoring
temperature, humidity & dehumidification
ultraviolet (UV) and ultraviolet C (UV-C)
face coverings
calculating required physical distances
calculating airflow
pressure zones
positive & negative pressure ventilation
turbulence
deposition rates
air walls
patient dedicated clean air supply methods, and
aerosolized SARS-CoV-2 transmission and COVID-19 infection risk estimators
Did you know that an airwall can be more effective than using solid barriers if properly placed and 2 people maintain safe physical distance?
Did you know that MERV 13 is commonly recommended by HVAC installation and maintenance businesses but the efficiency is a very low standard for infectious disease.
Did you know that there are two primary methods to model the risk of airborne infection. These models are based on entirely different mathematical and biostatistical models and produce very similar results.
Additional Resources
American Psychiatric Association Practice Guidance for COVID-19 (January 2021)
Coronavirus (COVID-19) Response Resources form ASHRAE and others
COVID-19 (2019 novel coronavirus) Resource Center for Physicians
Department of Labor – OSHA Guidance on Preparing Workplaces for COVID-19 (May 2020)
American Psychiatric Association Practice Guidance for COVID-19 (January 2021)
Steps Healthcare Facilities Can Take to Stay Prepared for COVID-19
(There is an underlying science and reasons that the above guidelines have in common.)
Disclaimer: The considerations for ethical practice presented in this paper are aspirational. They reflect basic ethical issues such as competence, do-no-harm, scope of practice, etc... This article does not replace or change any requirements established by a particular licensing board. Consult with your licensing board or an attorney regarding any questions you may have about specific differences.